Alopecia is the medical term for hair loss. Hair loss may occur naturally, or it may be related to a disease or the use of certain medications. Symptoms of alopecia vary depending on the cause of the condition and range from a small bald patch to a complete loss of all body hair.
Alopecia, commonly known as hair loss, is a medical condition characterised by the partial or complete loss of hair from the scalp or other areas of the body. It can affect individuals of all ages and genders, leading to various emotional and psychological challenges.
There are several types of alopecia, with the most common being Androgenetic Alopecia (male and female pattern baldness), caused by genetic and hormonal factors. Other forms include Alopecia Areata, an autoimmune disorder resulting in round, coin-sized patches of hair loss, and Telogen Effluvium, often triggered by stress or illness, causing excessive shedding.
Management and treatment options for alopecia vary, including medications, hair transplantation, and supportive hair loss treatments, depending on the underlying cause and severity of hair loss. Understanding the specific type of alopecia and seeking appropriate medical advice is crucial for effective management and potentially restoring one's confidence and self-esteem.
The Norwood scale (or Hamilton-Norwood scale) is a commonly used classification system used to measure the extent of male pattern baldness and ranges from stages 1 to 7. It provides easy-to-reference images that indicate different stages of balding.
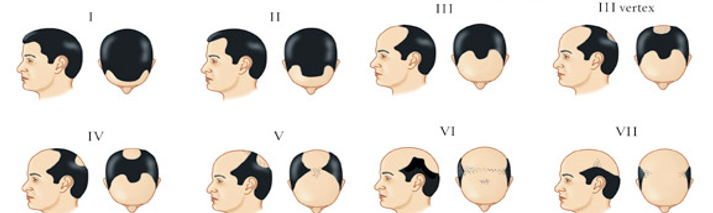
Norwood-Hamilton Scale of Male Pattern Baldness
The Ludwig scale is a method of classifying female pattern baldness (Androgenic Alopecia) and ranges from stages 1 to 3.
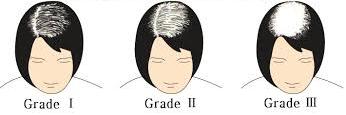
Ludwig Scale of Female Pattern Baldness
Understanding the intricacies of hair growth and loss is crucial for managing hair-related issues effectively. The hair growth cycle consists of three phases:
Understanding these aspects of hair growth and loss is pivotal in maintaining healthy locks. If you're concerned about hair loss, it's advisable to consult a dermatologist who can provide personalized guidance and treatment options. Early intervention can make a significant difference in preserving your hair's health and vitality.
This is a prevalent disorder that affects approximately 50% of men and many women (mostly older than 40 years). As many as 13% of premenopausal women reportedly have some evidence of Androgenetic Alopecia. This type of alopecia is commonly known as male pattern baldness or female pattern baldness. Thinning of hair occurs on the crown area, or hairline starts receding from the temples.
In most cases, hair continues to fall, leading to complete baldness with time. This progressive hair loss is believed to be due to genetic and hereditary factors.
Androgenetic alopecia, commonly known as male or female pattern baldness, is the most prevalent form of hair loss and is influenced by genetic, hormonal, and environmental factors.
It's important to consult with a dermatologist or hair specialist professional or DHI surgeons for a personalised assessment and treatment plan for androgenetic alopecia. Early intervention often yields better results in preserving and regrowing hair.



Hair loss due to scarring of the scalp is called scarring alopecia. Scarring can be due to a variety of causes. Traction alopecia over a period of time may lead to scarring and permanent hair loss. Similarly, trichotillomania (compulsive hair-plucking) can cause permanent scalp scarring over time. Injury to the scalp caused by physical trauma or burns may leave permanent scars and permanent hair loss. Diseases that may cause permanent hair loss due to scalp scarring include:
A form of scarring alopecia may also occur in post-menopausal women, associated with hair follicles’ inflammation and subsequent scarring.
Scarring alopecia, also known as cicatricial alopecia, is a type of hair loss characterized by permanent damage to hair follicles and the replacement of hair-bearing tissue with scar tissue. Its causes and risk factors can vary depending on the specific subtype of scarring alopecia, but common factors include:
Early diagnosis and prompt treatment are crucial to prevent further hair loss in cases of scarring alopecia, as hair follicles cannot regenerate once they are replaced by scar tissue.
The progression of Scarring Alopecia. Results are case-specific and are not guaranteed.
This type of alopecia occurs as round or oval hair loss patches, most obvious on the scalp or in the eyebrows. Those who develop these round or oval hair loss areas can progress to total scalp hair loss (Alopecia Totalis). The cause of Alopecia Areata is unknown but commonly believed to be an auto-immune disorder. The most common treatment is steroids (cortisone is one form), either topically or by injection.
Alopecia areata is an autoimmune disorder that causes hair loss, often in small, round patches on the scalp, although it can affect other body hair as well. The exact cause is not fully understood, but it is believed to involve a combination of genetic, environmental, and immune system factors. Risk factors and triggers include:


This refers to cases in which the scalp incurs complete hair loss. In an estimated 30% of patients, total hair loss occurs within six months after the disease’s onset.
It is an auto-immune disorder resulting in total hair loss, but on the scalp only. It is a condition intermediary between Alopecia Areata and Alopecia Universalis. Alopecia Totalis generally shows up in two types, the first being a relatively quick and complete hair loss in the head and the second being a slower type, which starts as a patchy loss (Alopecia Areata) and progresses to total hair loss in the scalp.
Alopecia totalis is a severe subtype of alopecia areata characterised by complete hair loss on the scalp.
While the precise cause remains uncertain, it is generally attributed to autoimmune factors and genetic predisposition. Risk factors for alopecia totalis include:
Consulting with a dermatologist is essential for accurate diagnosis and tailored treatment plans.
This is the most advanced and rare type of alopecia in which there is a complete loss of hair all over the body.
Alopecia universalis is an extreme form of alopecia areata, an autoimmune condition where the immune system mistakenly attacks hair follicles, resulting in hair loss. In alopecia universalis, hair loss extends to the entire body, including eyebrows, eyelashes, and body hair.
The exact causes remain unclear, but several factors and risk factors are associated with its development:
It's important to note that alopecia universalis is a complex condition with a multifactorial aetiology. Treatment options, including corticosteroids, immunosuppressive therapies, and topical medications, aim to manage the autoimmune response and stimulate hair regrowth, but results can vary among individuals. Consultation with a dermatologist or immunologist is crucial for proper diagnosis and personalised treatment.



Diffuse alopecia – also known as Alopecia Areata Incognita, is a rare form of alopecia and affects primarily young males, and the hair loss on the head is radical and sudden.
Diffuse alopecia, a condition characterised by widespread hair thinning or hair loss across the scalp can result from various underlying causes and risk factors. Understanding these factors is essential for effective diagnosis and management.
Identifying the specific cause of diffuse alopecia requires a thorough medical evaluation by a healthcare professional. Once the underlying factor is determined, appropriate treatment or management strategies, such as addressing the root cause, dietary changes, or medical therapies, can be implemented to help restore hair health.
When hair follicles are pushed prematurely in the hair growth cycle’s resting stage, the resulting hair loss is categorized as Telogen Effluvium.
Telogen effluvium is a temporary and diffuse hair loss condition characterised by a significant shedding of hair. Several risk factors can trigger telogen effluvium, including severe stressors like physical trauma, surgery, or emotional stress. Medical conditions such as thyroid disorders, anaemia, and chronic illnesses can also contribute to this hair loss condition. Nutritional deficiencies, crash diets, and rapid weight loss are additional risk factors. Medications, particularly those causing side effects like hair loss, are common culprits. Hormonal changes due to childbirth, menopause, or stopping birth control pills can trigger telogen effluvium as well. Identifying and addressing the underlying cause is key to managing this condition effectively.


This alopecia is usually caused due to excessive pulling or tension on hair shafts as a result of certain hairstyles.
The most common risk factor is tight hairstyles such as braids, cornrows, weaves, and tight ponytails. Excessive use of hair extensions and hair accessories that pull on the hair can also lead to traction alopecia. Frequent use of hot styling tools, chemical treatments, and improper hair care practices can weaken the hair shaft, making it more susceptible to damage. Additionally, individuals with naturally fine or fragile hair are at a higher risk of developing traction alopecia. Proper hair care and avoiding tight hairstyles are essential to prevent this condition.
Triangular alopecia, also known as temporal triangular alopecia or congenital triangular alopecia, is a rare and non-scarring form of hair loss that typically occurs in a well-defined triangular or oval-shaped area near the temples or frontal hairline. This condition primarily affects children and young adults but can persist into adulthood. While the exact cause of triangular alopecia remains unclear, it is believed to be a genetic disorder, as it often runs in families.
Loss of hair occurs in the temporal areas that sometimes begin in childhood. Hair loss may be complete, or a few fine, thin diameter hairs may remain. The cause of Triangular Alopecia is not known, but the condition can be treated medically or surgically.
Risk factors for triangular alopecia include a family history of the condition and the presence of other hair or scalp abnormalities. Clinical progression of this condition usually begins in childhood, with hair thinning or bald patches appearing near the temples. Over time, the affected area may expand, leading to more noticeable hair loss.
Treatment options for triangular alopecia are limited, and many individuals may choose to manage the condition with hairstyling techniques or hairpieces to conceal the affected area. In some cases, topical medications like minoxidil or hair transplantation may be considered to stimulate hair growth. Consulting a dermatologist can provide personalised guidance on managing triangular alopecia.
Alopecia, often referred to as hair loss, is a condition that affects millions of individuals worldwide. It can manifest in various forms, each with its own distinct characteristics and diagnostic methods.
Alopecia can be emotionally challenging, impacting self-esteem and body image. Coping strategies involve seeking support from friends, family, or support groups, as well as exploring hairpieces, wigs, or creative hairstyles to boost confidence. Embracing one's unique appearance and practising self-care are essential aspects of managing the emotional toll of alopecia.
Living with alopecia means adapting to a changing appearance and managing potential physical discomfort. It's important to prioritise self-acceptance, seek professional advice, and explore treatment options to address individual needs and preferences.
Alopecia encompasses a spectrum of conditions that can affect individuals of all ages and backgrounds. Understanding the type, seeking appropriate diagnosis, and exploring treatment options are crucial steps in managing alopecia effectively. Coping with the emotional impact and seeking support can make a significant difference in one's journey with hair loss. Ultimately, embracing individuality and self-acceptance are key to living a fulfilling life with alopecia.
Common types of alopecia include Alopecia Areata, Androgenetic Alopecia (male and female pattern baldness), Scarring Alopecia, Traction Alopecia, and Telogen Effluvium.
There is no universal cure for all types of alopecia. Treatment options vary depending on the specific type and may include medications, surgical procedures, or lifestyle changes to manage symptoms and promote hair regrowth.
Maintaining a balanced diet, managing stress, avoiding harsh hair treatments, and quitting smoking can support overall hair health. Specific lifestyle changes may be recommended based on the type and cause of hair loss.
Yes, alopecia can be hereditary. Genetic factors play a significant role in conditions like Androgenetic Alopecia, where family history is a key risk factor.
Alopecia can have profound emotional effects, including reduced self-esteem and body image concerns. Individuals may experience anxiety, depression, or social withdrawal. Seeking emotional support, counselling, and practising self-acceptance are essential in coping with these emotional challenges.